Aging is a natural part of life, and changes in memory and thinking are common as people get older. However, not all memory problems are the same. Some changes are a normal part of aging, while others may be warning signs of more serious conditions like mild cognitive impairment (MCI) or dementia, including Alzheimer’s disease. This handout will help explain the differences, what to watch for, and when to talk to a healthcare provider.
What Is Normal Aging?
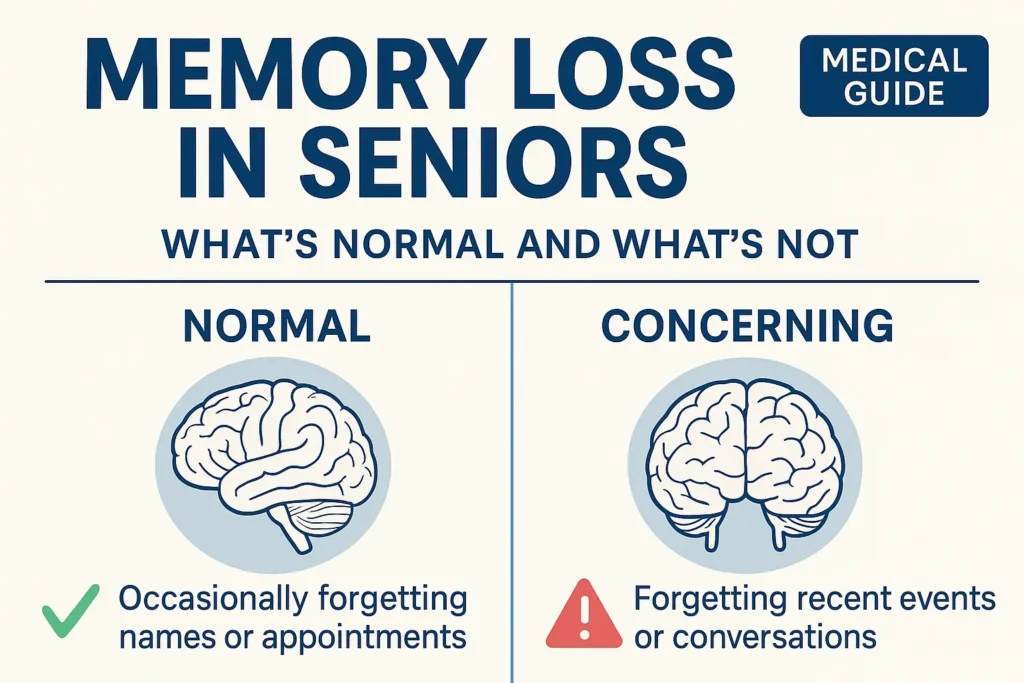
As people age, the brain changes just like the rest of the body. It’s normal to notice some mild changes in memory and thinking. Common examples include:
- Occasionally forgetting names or appointments, but remembering them later
- Misplacing items like keys or glasses from time to time
- Sometimes having trouble finding the right word
- Walking into a room and forgetting why
- Taking a bit longer to learn new things or recall information
These changes usually do not affect a person’s ability to live independently or do everyday activities. Most older adults can still manage their finances, medications, and household tasks, even if they need to write things down or use reminders.
What Are Warning Signs of Something More Serious?
Some memory problems are more than just normal aging. They may be signs of mild cognitive impairment (MCI) or dementia. These conditions involve more noticeable changes in thinking and memory, and sometimes affect daily life.
Related Post: How Vitamin B12 Can Help The Brain
Mild Cognitive Impairment (MCI)
MCI is a condition where a person has more memory or thinking problems than expected for their age, but can still do most daily activities on their own. People with MCI may:
- Forget important information, like recent conversations or appointments, more often than others their age
- Have trouble remembering recent events that would normally interest them (for example, a sports fan forgetting the outcome of a game)
- Notice these changes themselves, or have family and friends point them out
- Still manage their own finances, medications, and household tasks without help
MCI does not cause major problems with independence. However, it can be a warning sign, as some people with MCI go on to develop dementia. Others may stay the same or even improve.
Dementia
Dementia is a more serious condition. It means there are problems with memory and thinking that are severe enough to interfere with daily life. People with dementia may:
- Need help with basic activities, like bathing, dressing, or eating
- Get lost in familiar places or become confused about time or people
- Have trouble managing money, paying bills, or taking medications correctly
- Repeat the same questions or stories over and over, even within a short time
- Struggle to follow conversations or instructions
- Show changes in mood, personality, or behavior, such as becoming withdrawn, suspicious, or easily upset
Dementia is not a normal part of aging. It is caused by diseases that damage the brain, such as Alzheimer’s disease, vascular dementia (from strokes or blood vessel problems), or other conditions.
How Common Are These Conditions?
Mild cognitive impairment (MCI): About 1 in 5 people age 65 and older have MCI.
Dementia: About 1 in 7 people age 65 and older have dementia. The risk increases with age: about 3% of people ages 65–74, 10% ages 75–84, and nearly 30% ages 85 and older.
What Causes Memory Loss?
Many things can affect memory and thinking. Some are part of normal aging, but others are treatable medical problems. Common causes include:
Aging: Natural changes in the brain
Alzheimer’s disease: The most common cause of dementia
Vascular problems: Strokes or blood vessel disease
Medications: Some drugs can cause confusion or memory problems
Depression or anxiety: Can make it hard to concentrate or remember
Sleep problems: Poor sleep affects memory
Vitamin deficiencies: Low vitamin B12
Metabolic disease: hypothyroidism, hyperthyroidism
Chronic Liver disease
Hearing or vision loss: Can make it harder to process information
It’s important to talk to a healthcare provider if memory problems are new, getting worse, or affecting daily life. Some causes can be treated or improved.
How Do Doctors Tell the Difference?
Doctors use several steps to figure out if memory changes are normal or a sign of something more serious:
1. History and Questions: The doctor will ask about memory problems, when they started, and how they affect daily life. Family or friends may be asked for their observations.
2. Brief Memory Tests: Simple tests in the office, like asking questions or drawing a clock, can help check memory and thinking. Common tests include the Mini-Mental State Examination (MMSE), Montreal Cognitive Assessment (MoCA), and Mini-Cog.
3. Further Evaluation: If needed, more detailed tests, blood work, or brain scans may be done to look for treatable causes or to confirm a diagnosis.
4. Functional Assessment: Doctors may ask about daily activities, such as managing money, cooking, or shopping, to see if help is needed.
Doctors look for patterns: Is the person just a little forgetful, or are they having trouble with daily life? Are the changes getting worse? Are there other symptoms, like confusion or changes in mood?
What Are the Risk Factors for Memory Problems?
Some things make memory problems more likely as people age:
Age: The biggest risk factor
Family history: Having relatives with dementia
Heart and blood vessel problems: High blood pressure, diabetes, high cholesterol
Depression
Physical frailty
Low education or social support
Lifestyle factors: Poor diet, lack of exercise, smoking, heavy alcohol use
Some lifestyle choices may help lower the risk:
Eating a healthy diet (like the Mediterranean diet)
Staying physically active
Keeping the brain active (reading, puzzles, learning new things)
Staying socially connected
Managing health conditions (blood pressure, diabetes, cholesterol)
Getting enough sleep
Avoiding smoking and heavy drinking
When Should Someone Seek Help?
It’s important to talk to a healthcare provider if:
Memory problems are getting worse or are different from usual
There is trouble doing everyday tasks, like paying bills or taking medications
Getting lost in familiar places
Repeating questions or stories often
Changes in mood, personality, or behavior
Family or friends are concerned
Early evaluation can help find treatable causes, plan for the future, and connect to support and resources.
What Can Be Done?
While some memory changes are normal, there are steps to support brain health and possibly slow down decline:
Stay active: Regular exercise helps the brain and body
Eat well: A diet rich in fruits, vegetables, whole grains, and healthy fats
Keep learning: Challenge the brain with new activities
Stay social: Connect with friends and family
Manage health: Control blood pressure, diabetes, and cholesterol
Sleep well: Aim for good sleep habits
Avoid smoking and limit alcohol
Treat depression or anxiety: Mental health affects memory
If a diagnosis of MCI or dementia is made, doctors can help with treatment, planning, and support. New treatments for Alzheimer’s disease and other dementias are being developed, and early diagnosis may help people access these options.
What About Screening for Memory Problems?
Routine screening for memory problems in people without symptoms is not currently recommended by the United States Preventive Services Task Force or the American Heart Association. However, doctors should be alert for changes in memory or thinking, especially if patients or family members are concerned. Medicare covers a yearly wellness visit that includes a check of memory and thinking.