When most people hear the word “Botox,” they immediately think of cosmetic procedures the smooth foreheads and wrinkle-free faces that have become synonymous with anti-aging treatments. However, what many don’t realize is that “Botox,” which is a brand name for botulinum toxin, the active ingredient in Botox, has revolutionized the treatment of several debilitating neurological conditions.
Far from being merely a vanity product, botulinum toxin has emerged as a crucial therapeutic tool in neurology, offering relief to millions of patients suffering from chronic migraines, spasticity, and dystonia.
Botox Migraine Treatment Boca Raton
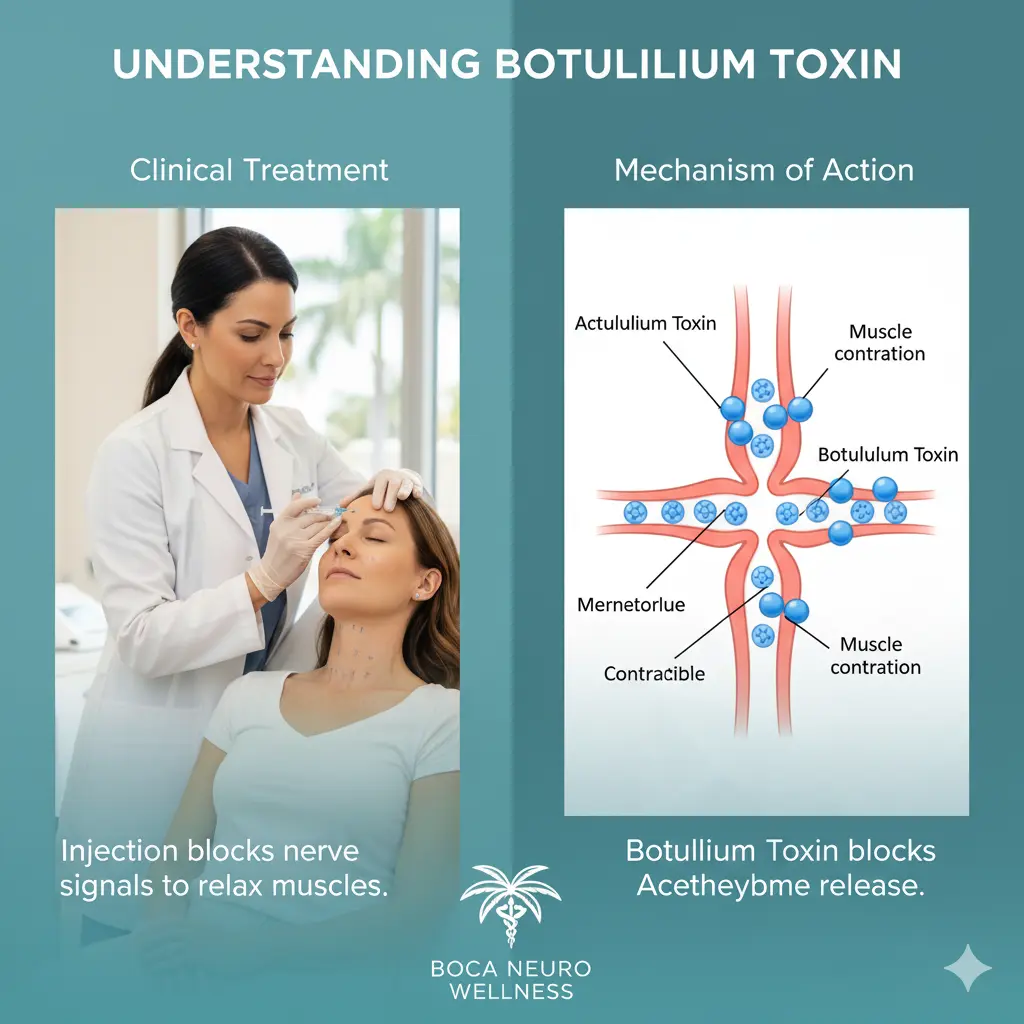
Botulinum toxin is produced by the bacterium Clostridium botulinum. While the toxin is potentially deadly in large amounts causing botulism, a serious form of food poisoning when purified and used in tiny, controlled doses, it becomes a powerful medical treatment.
The toxin works by blocking the release of acetylcholine, a neurotransmitter that signals muscles to contract. This blocking action temporarily paralyzes or weakens muscles, which proves therapeutic in conditions characterized by excessive muscle activity or abnormal nerve signaling.
There are several formulations of botulinum toxin available for medical use, with botulinum toxin (onabotulinumtoxinA) being the most well-known. Other formulations include Dysport, Xeomin, and Myobloc, each with slightly different properties and uses. The discovery that this toxin could be harnessed for medical benefit represents one of the most remarkable transformations in modern medicine turning a deadly poison into a healing agent.
Botulinum Toxin for Chronic Migraines
Chronic migraines affect approximately 2% of the global population, causing devastating impacts on quality of life, work productivity, and mental health. Unlike episodic migraines, which occur fewer than 15 days per month, chronic migraines are defined as headaches occurring on 15 or more days per month for at least three months, with at least eight of those days featuring migraine characteristics.
The journey to using botulinum toxin for migraines began somewhat serendipitously. In the late 1990s, physicians noticed that patients receiving cosmetic botulinum toxin injections reported fewer headaches. This observation sparked clinical investigations that eventually led to FDA approval of botulinum toxin for chronic migraine prevention in 2010.
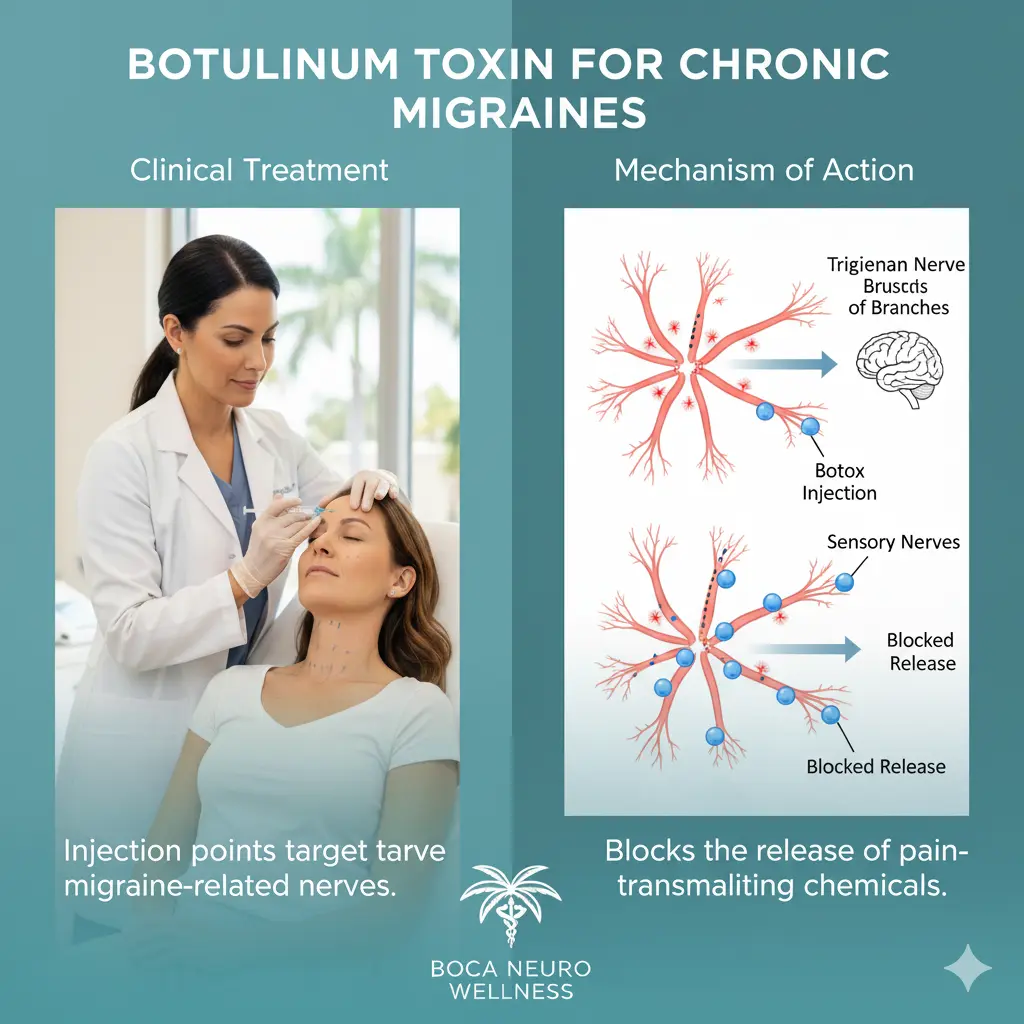
The mechanism by which botulinum toxin prevents migraines is not entirely understood, but it appears to work differently than its muscle-paralyzing effects. Researchers believe that botulinum toxin inhibits the release of pain neurotransmitters and inflammatory substances from nerve endings.
It essentially interrupts the pain pathways before they can fully activate, preventing the cascade of events that leads to a migraine attack. The toxin may also reduce peripheral sensitization of pain nerves, making them less likely to trigger the central nervous system changes associated with migraines.
The treatment protocol for chronic migraines involves injecting small amounts of botulinum toxin into specific areas around the head and neck. A typical treatment consists of 31 injections across seven key areas: the forehead, temples, back of the head, neck, and shoulders. Each injection site receives approximately 5 units of botulinum toxin, for a total of 155 units per treatment session. The procedure takes about 15 minutes and is performed in an outpatient setting.
Patients don’t experience immediate relief. It typically takes 10 to 14 days for the effects to begin, with maximum benefit often occurring around the four-week mark. Treatments are repeated every 12 weeks, as the effects gradually wear off. Clinical trials have shown that botulinum toxin can reduce the number of headache days per month by approximately 8 to 9 days a significant improvement that can dramatically enhance a patient’s quality of life.
Not every patient responds equally to botulinum toxin treatment. Studies suggest that about 70% of chronic migraine patients experience meaningful improvement. Some patients become nearly headache-free, while others see more modest reductions. Factors that may predict better outcomes include the absence of medication overuse headaches, shorter duration of chronic migraines, and younger age at treatment initiation.
The side effects of botulinum toxin for migraines are generally mild and temporary. These may include neck pain, muscle weakness, drooping eyelids, and injection site discomfort. Serious complications are rare when the treatment is administered by experienced practitioners.
For many patients who have tried and failed multiple preventive medications, or who cannot tolerate oral preventives due to side effects, botulinum toxin offers a valuable alternative with a different side effect profile.
Botulinum Toxin for Spasticity
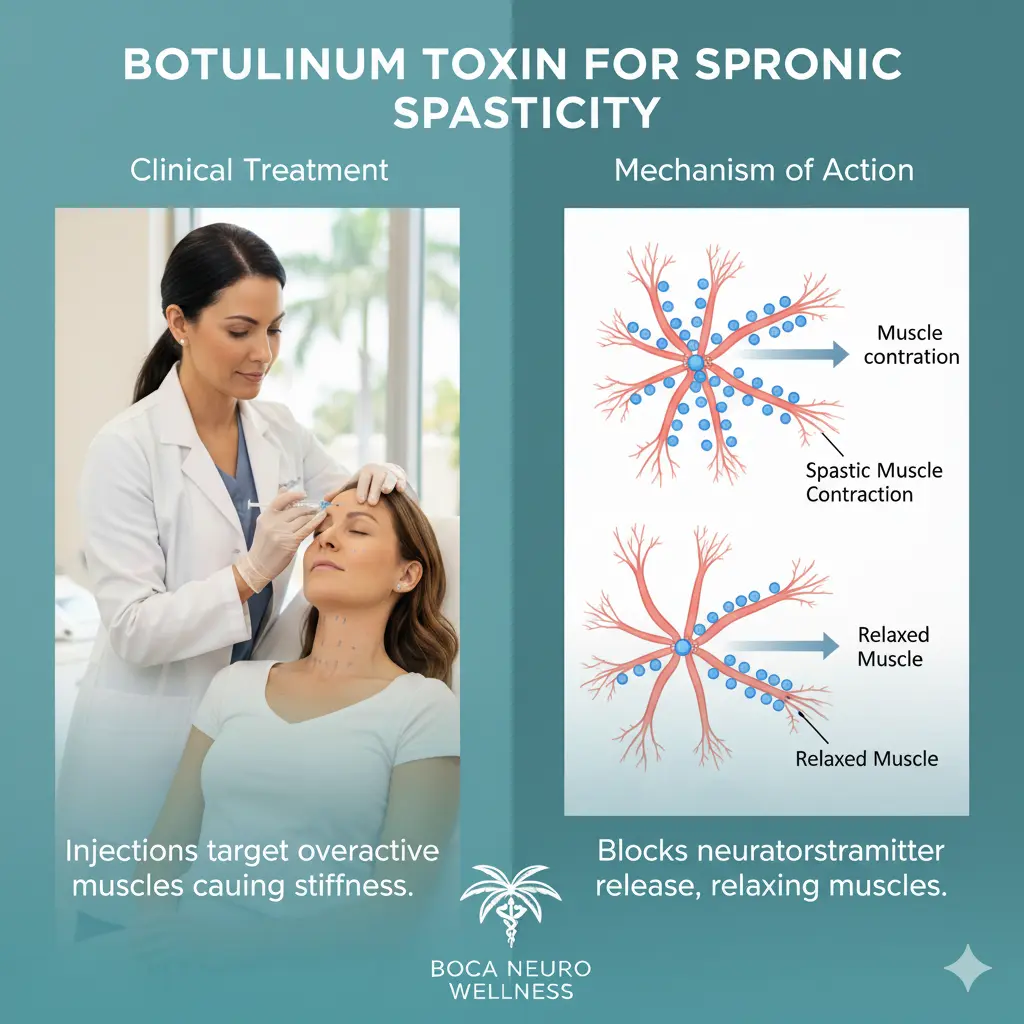
Spasticity is a condition characterized by abnormal muscle stiffness, tightness, and involuntary spasms. It results from damage to the brain or spinal cord that disrupts the nerve signals controlling muscle movement. Common causes include stroke, multiple sclerosis, cerebral palsy, traumatic brain injury, and spinal cord injury. Spasticity can significantly impair mobility, cause pain, interfere with daily activities, and lead to complications such as contractures (permanent muscle shortening) and pressure sores.
Botulinum toxin was first approved for treating spasticity in the upper limbs following stroke in 2010, and subsequently for lower limb spasticity in adults in 2016. It has also been approved for treating spasticity in children with cerebral palsy.
The treatment approach involves injecting botulinum toxin directly into the spastic muscles. By blocking acetylcholine release at the neuromuscular junction, botulinum toxin reduces the excessive muscle tone that characterizes spasticity. This allows for improved range of motion, reduced pain, easier care and hygiene, and better function. The effects begin within a few days to two weeks and last approximately three to six months.
One of the key advantages of botulinum toxin for spasticity is its targeted action. Unlike oral antispasticity medications like baclofen or tizanidine, which affect the entire body and can cause sedation and weakness, botulinum toxin allows physicians to treat specific problematic muscles while leaving others unaffected. This precision is particularly valuable when spasticity is localized or when patients need to maintain strength in certain muscle groups.
The treatment is often most effective when combined with physical therapy. After botulinum toxin reduces muscle tone, therapists can work more effectively on stretching, strengthening, and retraining movement patterns. This combination approach known as chemodenervation plus rehabilitation often produces better functional outcomes than either treatment alone.
Determining which muscles to inject and how much botulinum toxin to use requires considerable expertise. Neurologists often use electromyography (EMG) guidance or electrical stimulation to precisely locate the muscles contributing most to spasticity. The total dose varies depending on the number and size of muscles treated, but healthcare providers must stay within safe maximum doses to avoid complications.
For many patients with spasticity, botulinum toxin has been truly transformative. A stroke survivor who couldn’t open their clenched fist due to severe arm spasticity may regain the ability to grasp objects. A child with cerebral palsy might walk more easily after treatment of leg spasticity. These functional improvements can enhance independence, reduce caregiver burden, and improve overall quality of life.
Botulinum toxin for Dystonia
Dystonia is a movement disorder characterized by sustained or intermittent muscle contractions that cause abnormal, often repetitive movements, postures, or both. The condition can affect a single body part (focal dystonia), two or more adjacent parts (segmental dystonia), or the entire body (generalized dystonia). Dystonia can be primary (occurring without an identifiable cause) or secondary to other conditions such as Parkinson’s disease, brain injury, or certain medications.
Cervical dystonia (also called spasmodic torticollis) is the most common focal dystonia in adults. It affects the neck muscles, causing the head to twist or turn to one side, tilt forward or backward, or pull toward the shoulder. The condition is often painful and can be socially isolating due to the visible abnormal postures.
Botulinum toxin was actually first approved for a neurological condition when it received FDA approval for cervical dystonia in 2000. This approval marked a watershed moment in recognizing the therapeutic potential of botulinum toxin beyond cosmetics.
The mechanism of action for dystonia treatment is straightforward: by weakening the overactive muscles responsible for the abnormal movements or postures, botulinum toxin helps restore a more normal position and reduces associated pain. However, achieving the right balance requires skill. Injecting too little may provide inadequate relief, while injecting too much can cause excessive weakness and difficulty with normal movements like swallowing or holding the head up.
Treatment typically involves injecting several neck muscles based on the specific pattern of dystonia. The effects begin within a few days to two weeks and last approximately three to four months. Patients usually require repeated treatments indefinitely, as the condition itself doesn’t resolve.
Studies have consistently shown that botulinum toxin significantly reduces both the severity of abnormal postures and associated pain in cervical dystonia. Many patients experience dramatic improvements that allow them to return to work and social activities. The treatment has become the first-line therapy for this condition, with oral medications typically reserved for cases where botulinum toxin alone provides insufficient benefit.
Beyond cervical dystonia, botulinum toxin is used for other focal dystonias including blepharospasm (involuntary eyelid closure), oromandibular dystonia (affecting jaw and mouth muscles), spasmodic dysphonia (affecting voice box muscles), and limb dystonias. Each type requires specialized injection techniques and knowledge of the relevant anatomy.
Writer’s cramp, a task-specific dystonia affecting the hand during writing, and musician’s dystonia, affecting fingers during instrument playing, are particularly challenging to treat. These require extremely precise injections to weaken problematic muscles while preserving the fine motor control needed for these skilled activities.
Safety and Considerations
Across all neurological applications, botulinum toxin has demonstrated a strong safety profile when used appropriately. The most common side effects relate to the specific injection sites and include pain, bruising, and temporary weakness of nearby muscles. Rarely, the toxin can spread beyond the injection site, causing symptoms like difficulty swallowing, breathing problems, or generalized weakness. These serious complications are extremely uncommon with proper dosing and technique.
Certain populations should not receive botulinum toxin, including pregnant or breastfeeding women, people with neuromuscular diseases like myasthenia gravis or ALS, and those allergic to any ingredient in the formulation. A thorough medical evaluation is essential before starting treatment.
The cost of botulinum toxin treatment can be substantial, but most insurance plans cover it for approved neurological indications when medical necessity is documented. Prior authorization is typically required, and patients may need to try and fail other treatments first.
The Future of Botulinum Toxin in Neurology
For the millions of people living with chronic migraines, spasticity, or dystonia, botulinum toxin represents hope not for wrinkle reduction, but for reduced pain, improved function, and enhanced quality of life. As our understanding of botulinum toxin’s mechanisms continues to grow, so too will its applications, potentially offering relief to even more patients in the future.