Neuropathy, broadly defined, refers to disorders affecting the peripheral nervous system the network of nerves outside the brain and spinal cord. These nerves transmit sensory, motor, and autonomic signals between the central nervous system and the rest of the body.
Neuropathy can manifest as a wide spectrum of symptoms, ranging from numbness and tingling to weakness, pain, and autonomic dysfunction. The condition is common, affecting 1% to 7% of the general population, with prevalence increasing with age and in those with chronic diseases such as diabetes mellitus.
Types and Classification of Neuropathy
Neuropathy is classified by the pattern of nerve involvement, the type of nerve fibers affected, and the underlying etiology. The most common form is distal symmetric polyneuropathy (DSP), which typically presents with symptoms in a “stocking and glove” distribution starting in the feet and hands and progressing proximally.
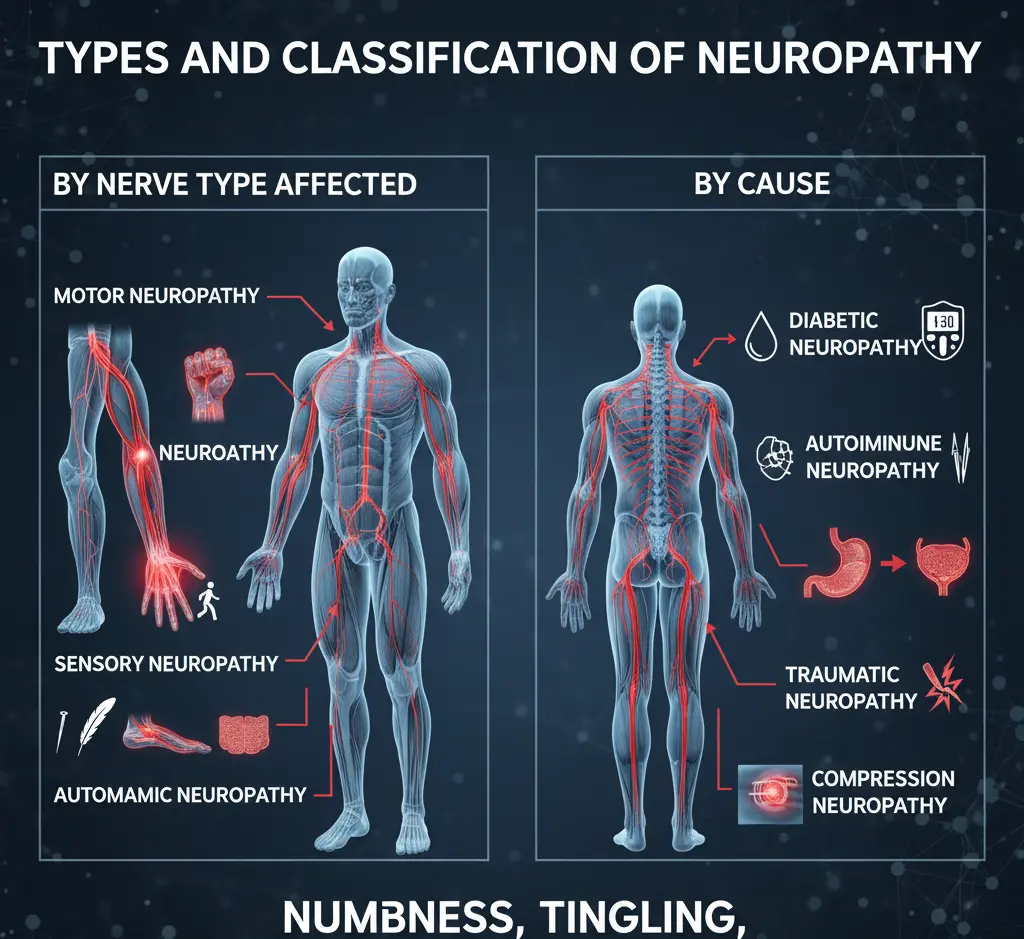
Other forms include mononeuropathy (single nerve involvement), mononeuropathy multiplex (multiple individual nerves), and small-fiber or large-fiber neuropathies, depending on the affected nerve fibers.
• Sensory neuropathy affects sensation, leading to numbness, tingling, burning, or pain.
• Motor neuropathy impairs muscle function, causing weakness or atrophy.
• Autonomic neuropathy disrupts involuntary functions, such as blood pressure regulation, sweating, and gastrointestinal motility.
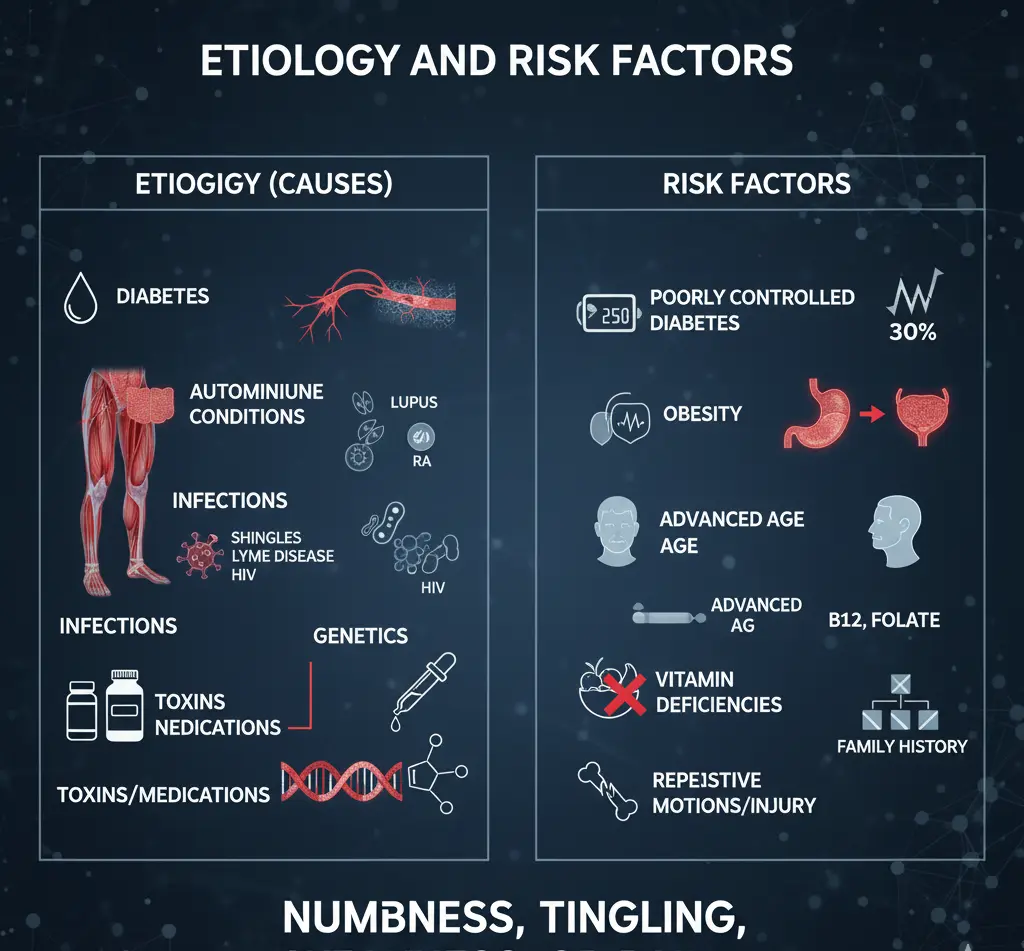
Etiology and Risk Factors
Neuropathy has numerous causes, with diabetes mellitus being the most common in developed countries. Other causes include:
• Metabolic disorders: Diabetes, hypothyroidism, renal failure.
• Nutritional deficiencies: Vitamin B12, folate.
• Toxins: Alcohol, certain medications (e.g., chemotherapy, antiretrovirals).
• Infections: HIV, Lyme disease.
• Hereditary diseases: Charcot-Marie-Tooth disease.
• Immune-mediated conditions: Guillain-Barré syndrome, chronic inflammatory demyelinating polyneuropathy (CIDP).
• Idiopathic: Up to 46% of cases have no identifiable cause after standard evaluation.
Clinical Presentation
The symptoms of neuropathy depend on the nerves and fibers involved. Early symptoms often include sensory changes numbness, tingling, burning, or pain typically in the feet. As the disease progresses, symptoms may ascend to the legs and hands. Motor involvement may present as weakness, muscle wasting, or difficulty with fine motor tasks. Autonomic symptoms can include orthostatic hypotension, abnormal sweating, gastrointestinal disturbances, and sexual dysfunction.
Physical Examination
A thorough neurologic and musculoskeletal examination is essential. Key components include:
• Sensory testing: Pinprick, temperature, vibration (using a 128-Hz tuning fork), and monofilament testing for protective sensation.
• Motor assessment: Muscle strength, tone, and bulk.
• Reflexes: Deep tendon reflexes, often reduced or absent in neuropathy.
• Autonomic evaluation: Blood pressure changes, skin changes, and other signs of autonomic dysfunction.
Diagnostic Approach
The diagnostic evaluation of neuropathy begins with a comprehensive history and physical examination. The goal is to identify treatable causes and characterize the pattern of neuropathy. Initial laboratory tests should include:
• Complete blood count
• Comprehensive metabolic panel@
• Fasting blood glucose and glucose tolerance test
• Vitamin B12 level
• Thyroid-stimulating hormone
• Serum protein electrophoresis with immunofixation
Additional tests may be indicated based on clinical suspicion, such as testing for HIV, Lyme disease, or autoimmune markers. Electrodiagnostic studies (nerve conduction studies and electromyography) are useful for distinguishing axonal from demyelinating neuropathies and for confirming the diagnosis in atypical cases.
EMG/Nerve conduction studies serve to:
1. Identify or confirm the presence of neuropathy
2. Assess the severity of the neuropathy
3. Determine the type of neuropathy (axonal, demyelinating, sensory and/or motor predominance). Treatment can be very different based on the type of neuropathy that is identified (such as treating demyelinating neuropathies with gammaglobulin).
When to See a Neurologist in Boca Raton, Florida?
Many cases of typical distal symmetric polyneuropathy can be managed in primary care with limited laboratory testing. However, referral to a neurologist in Boca Raton, Florida is appropriate when:
• Atypical features are present: Asymmetry, non–length-dependent distribution, motor predominance, acute or subacute onset, or prominent autonomic involvement.
• Rapid progression or severe weakness: Suggests a potentially treatable or reversible cause.
• Diagnosis is unclear after initial workup: Especially if initial laboratory tests are inconclusive.
• Suspected hereditary, immune-mediated, or rare causes: May require specialized testing or management.
• Need for advanced diagnostic procedures: Electrodiagnostic studies, nerve or skin biopsy, or genetic testing.
• Significant or difficult-to-manage neuropathic pain.
Management Principles
Treatment of neuropathy focuses on three main areas:
1. Addressing the underlying cause: Tight glycemic control in diabetes, correcting nutritional deficiencies, discontinuing neurotoxic medications, treating infections, or managing autoimmune conditions.
2. Symptomatic management: Neuropathic pain is often treated with medications such as gabapentinoids (gabapentin, pregabalin), tricyclic antidepressants, serotonin-norepinephrine reuptake inhibitors (duloxetine, venlafaxine), and topical agents. Opioids are generally avoided due to risk of dependence and limited efficacy.
3. Prevention of complications: Regular foot care, fall prevention strategies, and monitoring for ulcers or infections, especially in diabetic patients.
Diabetic Neuropathy: A Special Focus
Diabetic peripheral neuropathy (DPN) is the most common cause of neuropathy worldwide. The American Diabetes Association recommends annual screening for DPN in all patients with type 2 diabetes and those with type 1 diabetes of five years’ duration or longer. Early symptoms often involve pain and dysesthesia due to small-fiber involvement, while large-fiber involvement leads to numbness, loss of protective sensation, and increased risk of foot ulceration.
Clinical tests for DPN include pinprick and temperature sensation (small fibers), vibration and monofilament testing (large fibers), and assessment of protective sensation. Electrophysiological testing or referral to a neurologist is rarely needed unless atypical features are present.
Prognosis and Complications
The prognosis of neuropathy depends on the underlying cause and the timeliness of intervention. Some forms, such as those due to nutritional deficiencies or certain immune-mediated conditions, may be reversible if treated early. Chronic neuropathy can lead to significant morbidity, including pain, falls, foot ulcers, and amputations. Get Expert Neuropathy Care in Boca Raton.
Conclusion
Neuropathy is a common and potentially disabling condition with diverse etiologies and clinical presentations. Early recognition, appropriate diagnostic evaluation, and timely intervention are critical to prevent irreversible damage and improve quality of life.
Most cases of typical distal symmetric polyneuropathy can be managed in primary care, but neurologist referral is warranted for atypical presentations, rapid progression, diagnostic uncertainty, or suspected rare causes. Ongoing research continues to refine diagnostic strategies and expand treatment options, with the goal of improving outcomes for patients with neuropathy. Schedule Your Treatment top neurologist in boca raton, neuro doctor near you.